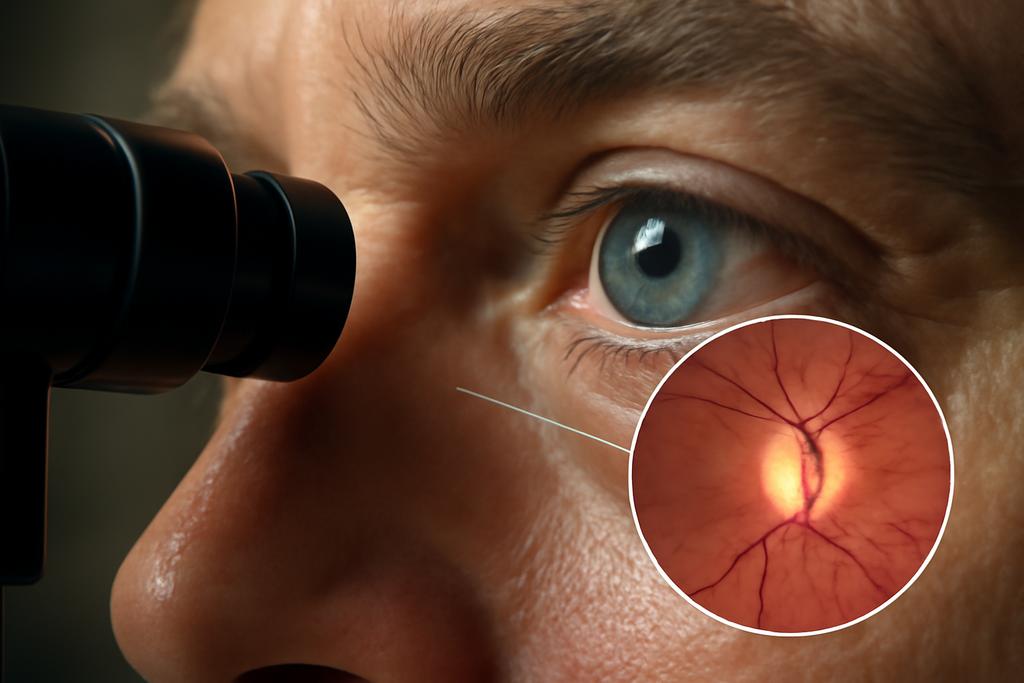
Our eyes are more than lenses and light traps; they’re living sculptures, flexing under pressure as if tiny pressure-cookers held in a delicate glass globe. Glaucoma, one of the leading causes of irreversible blindness, latches onto that tension and reshapes the optic nerve head in ways we’re only starting to understand. A new line of work from researchers at the University of Pittsburgh and Harvard Medical School asks a provocative question: which parts of the eye actually matter when we model its mechanics, and what does that mean for diagnosing and understanding glaucoma?
The study, led by Soumaya Ouhsousou of Pitt with collaborators at Harvard’s Mass Eye and Ear and Schepens Eye Research Institute, uses real, in vivo imaging to build subject-specific mechanical models of the eye. It’s not just about pretty pictures; it’s about turning imaging data into simulations that tell us which tissues contribute most to how the optic nerve head deforms under pressure. The core insight is both surprisingly pragmatic and surprisingly human: you don’t need every tissue to get the job done—what’s essential can be identified, saved from complexity, and still capture the brain’s story about glaucoma risk.
Think of it like urban planning for the eye. If you want to predict where stress concentrates in a city, you don’t need a full map of every storefront. You need the major arteries, the main barriers, and the critical chokepoints. This work asks: which ocular tissues are the big traffic drivers when the eye is pressed from inside (intraocular pressure) and by the fluid surrounding the brain (intracranial pressure)? The answer matters because better models could guide how we interpret imaging, design therapies, and ultimately protect vision for people at risk of glaucoma.
What the Eye Model Teaches Us About Real Life
To build their subject-specific eye geometries, the researchers drew on swept-source optical coherence tomography (SS-OCT) scans from two healthy men in their 60s and early 70s. They reconstructed three-dimensional shapes of the retina, choroid, sclera, lamina cribrosa (the mesh-like gateway through which the retinal nerve fibers pass), and the optic nerve itself. The posterior boundary of the lamina cribrosa isn’t always visible in scans, so the team filled in those gaps using carefully chosen “standard” dimensions from the literature. Then they wrapped the ONH inside a hollow sphere representing the eyeball, with a realistic, subject-specific axial length estimate. It’s a kind of digital, living eye—one that can be pressed by fluid pressures and watched respond in a computer lab rather than a physical lab bench.
The modeling relied on finite element analysis, a toolbox engineers use to simulate how materials deform under forces. They treated some tissues as linear elastic and others as hyperelastic, chosen to reflect what scientists know about how different eye tissues behave. The aim wasn’t to nail a perfect, tissue-by-tissue match for every subject, but to ask a sharper question: which tissue regions are indispensable for accurately capturing the mechanics of the optic nerve head? The team performed a battery of sensitivity tests—changing tissue stiffness and even removing whole tissue regions in silico—to see how much those choices would sway the predicted strains in the lamina cribrosa, retina, and optic nerve under normal IOP (about 20 mmHg) and ICP (about 10 mmHg) conditions, then under pressure changes. The results guided a curated, minimal-but-robust set of tissues for the final modeling approach.
One of the study’s signature moves is its insistence on in vivo subject specificity. Previous work often leaned on generic eye shapes or ex vivo tissues, but here the geometry and material properties were anchored in living imaging data. The lead authors show a quiet confidence: the math can matter less than the anatomy if you respect the anatomy that actually governs the mechanical behavior. And that matters because glaucoma research has long suffered from inconsistent, sometimes contradictory predictions about how pressure translates into strain in the lamina cribrosa. If you can standardize the essential geometry and tissue choices, you stand a better chance of comparing apples to apples across patients and studies.
Which Tissues Move the Lamina Cribrosa the Most
The team’s first big finding is a practical one: not all ocular tissues push the lamina cribrosa (LC) in equal measure. By systematically tweaking the stiffness of each region, they quantified how much the LC’s surface and interior strains shifted. The sclera—the eye’s tough outer shell—carried the heaviest weight. Its stiffness had the largest, most consistent effect on LC strains, dwarfing even the LC’s own material properties. In other words, the eye’s outer wall acts like a strong drumhead; when you tighten or loosen it, the LC’s response to pressure changes dramatically.
Second in line was the dura mater, one of the stiffest tissues surrounding the optic nerve, followed by the pia mater, the delicate sheath hugging the nerve itself. These two layers transmit the cerebrospinal fluid pressure into the optic nerve complex, shaping how pressure variations reach the LC. The optic nerve’s own stiffness also mattered—when the nerve was more compliant, the LC experienced higher tensile strains under the same pressure, and when the nerve was stiffer, the strains shifted differently. It’s a reminder that the LC doesn’t live in isolation: it’s part of a mechanical ecosystem, with each component speaking to the others through the shared load of pressure and structure.
Beyond these heavy hitters, a cluster of other tissues—the Bruch’s membrane, border tissue, annular ring, and Bruch’s membrane again—exerted only a small effect on LC mechanics in the simulations. Their influence hovered around a few percent at most. The retina itself, surprisingly, had a relatively modest effect on LC strains once you keep the retina’s behavior within plausible bounds, even though it’s the tissue that directly faces the inward push of IOP. The take-home message is starkly practical: if you want to build a robust LC model, you prioritize scleral stiffness, the LC itself, and the surrounding stiff layers (dura and pia), while you can afford to simplify or even exclude some thinner, peripheral tissues without sacrificing predictive power in the LC’s mechanics.
To illustrate the point about necessity, the authors ran binary tests: remove a tissue and watch how LC strains change. Removing Bruch’s membrane barely budged LC strains; removing border tissue or annular ring shifted the LC’s load pathways enough to matter, especially in the nasal and superior regions. Most telling: pia mater’s removal changed how the LC deformed under cerebrospinal fluid pressure, underscoring its role as a bridge between intracranial forces and the eyeball’s interior. All of this is more than a map-reading exercise. It provides a principled recipe for building subject-specific ONH models that are both accurate and computationally efficient, a feat that matters when you want to bring this approach toward clinical or large-scale research use.
Pressure as the Puppet Master
Pressure dynamics are at the heart of glaucoma’s puzzle, and this study pushes the narrative forward by combining intraocular pressure (IOP) and intracranial pressure (ICP) in a single, cohesive model. The researchers tested three IOP levels (10, 20, and 30 mmHg) and three ICP levels (5, 10, and 15 mmHg) to see how the lamina cribrosa would respond. Across the board, higher pressures nudged LC strains upward, but the spatial pattern of those strains mattered. The temporal (toward the temple) and inferior (toward the bottom) LC sectors consistently showed higher strains, a pattern that echoes clinical imaging studies in glaucoma and in healthy eyes under stress.
What makes the results especially compelling is the nuanced interaction between IOP and ICP. Increases in ICP amplified LC deformation, but the effect wasn’t uniform. The nasal and superior LC regions, for instance, exhibited the steepest increases in both tensile and compressive strains as ICP rose, while other regions showed more modest changes. This regional sensitivity aligns with clinical observations that glaucoma damage often has regional predilections, and it offers a mechanistic explanation: the translaminar pressure gradient—the difference between IOP and ICP—doesn’t just scale strain uniformly; it reshapes how load travels through the LC’s subregions.
As the authors point out, there is some debate in the literature about how ICP modulates LC mechanics. Some ex vivo or generic-model studies have found opposite trends. The in vivo, subject-specific approach here helps resolve part of that tension by showing clear, reproducible patterns when the same geometry and material assumptions are used across two living eyes. The upward trend of LC strains with rising ICP is consistent with several in vivo and donor studies, even if the magnitude of change varies with geometry, tissue anisotropy, and the specifics of boundary conditions. The bottom line is a cautious but hopeful one: recognizing ICP’s role—and its regional fingerprint on the LC—could refine how we interpret imaging signals and track glaucoma risk in individual patients.
Why a Robust Model Could Change Glaucoma Research
The most exciting upshot isn’t a new device or a single diagnostic trick; it’s a blueprint for more consistent, comparable science. By identifying a minimal yet sufficient set of tissues needed to faithfully simulate ONH mechanics, the study reduces the fog around what to include in subject-specific models. That matters because researchers have wrestled with wildly different modeling choices for the past decade: how many tissue layers to simulate, what material properties to assign, whether to treat tissues as isotropic or anisotropic, how to boundary the eye within a virtual globe. When those choices diverge, so too do the predicted strains in the LC and, by extension, hypotheses about glaucoma risk and progression.
Reducing this variability can accelerate progress in several ways. Clinically, improved, patient-specific models could augment risk stratification for glaucoma, offering a biomechanical lens to interpret imaging results alongside standard metrics like nerve fiber layer thickness. In research, a standardized approach means that studies can be compared more reliably, facilitating meta-analyses and cross-center collaborations. And for the broader public, the idea that a few structural powerhouses—the sclera, dura, pia, and LC—dominate the mechanical conversation helps translate a daunting body of biomechanics into something a bit more tangible: the eye’s outer framework and its immediate neighbors guide how pressure reshapes the optic nerve.
Of course, no model is a perfect crystal. The authors acknowledge limitations, such as assuming isotropy in most tissues and relying on a small number of in vivo subjects. They also note the challenge of capturing subject-specific tissue properties in living people. Future work could introduce anisotropy and viscoelastic behavior, expand the subject pool, and refine geometry as imaging technologies improve. If those steps pay off, we could move from static snapshots to dynamic, personalized biomechanical portraits of the eye—ones that help clinicians anticipate how glaucoma might unfold for a given patient and tailor interventions accordingly.
Beyond glaucoma, the study’s methodological core—how to discern which tissues truly matter in a complex mechanical system—has resonance for other parts of medicine and bioengineering. It’s a reminder that in living systems, the most influential players aren’t always the loudest or most obvious; sometimes the strongest influence comes from the structural backbone that you only notice when it’s not there. The paper’s authors—affiliated with the University of Pittsburgh’s Department of Civil and Environmental Engineering and Harvard Medical School’s ophthalmology groups—stand as a reminder that interdisciplinary work can translate delicate, image-rich science into the practical habit of asking the right questions about what to simulate and what to simplify.
In the end, the study’s approach—careful, tissue-level curation combined with patient-specific geometry—offers a compelling path forward. It’s a way to turn a messy, multi-tissue structure into a workable model that respects real-world anatomy and yields actionable insights. If glaucoma research can ride this methodological wave, we may not avoid the disease, but we can know it better, predict it earlier, and design smarter ways to protect vision longer.
Lead authors from the study emphasize that the sclera’s stiffness, the LC’s own properties, and the pia and dura mater around the optic nerve are the real levers in ONH mechanics. This isn’t a sensational headline about a miraculous new therapy; it’s a sober, practical refinement of how we study the eye’s response to pressure. And in a field where small differences in modeling choices have produced big swings in results, that clarity is a rare kind of signal worth listening to.
As the authors noted, the data and models are available from the corresponding author upon reasonable request, inviting other labs to test, reproduce, and extend these findings. That openness matters as much as the science itself, because glaucoma is a global challenge and understanding its biomechanics is a shared enterprise. The two-subject in vivo demonstration is just the opening move in a longer conversation about how we model eyes, measure risk, and protect sight for millions who live with—or are at risk for—glaucoma.